Source: CNN

Corinne Jameson-Kuehl, RDH, Owner Custom Dental Solutions
Measles is considered an acute respiratory illness. Because it is viral in nature, the common initial signs of possible infection include malaise, slight fever, and a loss of appetite. Patients are considered contagious four days before and four days after the rash appears. The virus is transmitted by airborne droplets when an infected person coughs, sneezes, or even breathes, making it one of the most highly contagious infectious diseases. Simply being in the same room with an infected person (and even up to two hours after they leave the area) means you are at risk for infection.
As dental practitioners, we need to be aware that the first visible signs of the disease are found in the head and neck. An infected patient will have a high fever, cough, runny nose, and conjunctivitis. A rash will form starting at the forehead and spread down to the trunk and feet. Koplik's spots may occur on the inside of the cheeks. These spots will appear small and whitish with a red background. It can be very dangerous for babies and children to be infected, as the disease can lead to pneumonia, deafness, and even brain damage in some cases.
Vaccinations
If unvaccinated providers believe they have been exposed, the CDC states that they can still receive the MMR (mumps, measles, and rubella) vaccination within 72 hours of exposure, followed up with an immunoglobulin treatment six days after vaccination.
“We need to be aware that the first visible signs of the disease are found in the head and neck.”
There are no specific antivirals. However, in severe cases, vitamin A is used in medical settings to help relieve symptoms for children. It is recommended that children receive two doses of the MMR vaccination at 12 months to 15 months and again from ages 4 to 6 years. Infants traveling to another country should have one dose before leaving the U.S.
Your provider-patient medical interview and written medical histories should include the following questions:
- Have you been vaccinated against measles?
- Have you traveled abroad recently (specifically to Europe, Asia, Pacific Islands, or Africa)?
- Have you or a family member been exposed to someone who has traveled abroad?
- Are you in a community where you suspect there could be a measles outbreak?
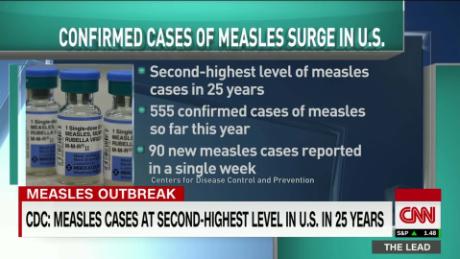
With more and more unvaccinated children and most U.S. cases being reported as being infected by an out-of-country exposure, it is imperative to continue with these questions chairside. If you find your office in the situation in which you believe there has been a measles exposure, the CDC asks that you to immediately report the suspected measles case to your local health department.




